
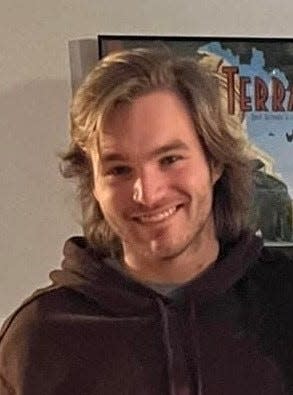
Cole Schmidtknecht, 22, of Appleton, died Jan. 21, 2024 of complications of an asthma attack. His parents are suing Walgreens and OptumRx, alleging the companies were negligent in raising the cost of the inhaler Schmidtknecht needed to $539.19 and offering him no alternative when he tried to refill his prescription.
A company being sued by a family for the death of their 22-year-old son who couldn’t afford his asthma inhaler is asking a judge to dismiss the lawsuit.
The parents of Cole Schmidtknecht, an Appleton man who died in January 2024 after suffering a severe asthma attack just days after his family says he stopped using his preventative inhaler due to a severe price hike, filed a lawsuit last month against OptumRx, a subsidiary of UnitedHealth Group, and Walgreens.
In the lawsuit complaint, Cole’s parents, Bil and Shanon Schmidtknecht, allege both OptumRx and Walgreens were negligent and bear responsibility for their son’s death. Five days before Cole’s catastrophic asthma attack, he went to his pharmacy, the Walgreens at 729 Northland Ave. in Appleton, to refill his prescription. There, he learned his inhaler — which he had been taking daily as a preventative medication to manage his asthma for around 10 years, his parents said — was no longer covered by his insurance, and now cost him nearly $540. Unable to afford it, Cole left the pharmacy with only a rescue inhaler he was able to get with a $5 copay.
Cole’s parents allege OptumRx discontinued coverage of Cole’s inhaler, Advair Diskus, in a decision that was financially and not medically motivated, then never provided the 30-day notice of the coverage change that is required by state law. The lawsuit complaint further alleges that Walgreens employees did not take any steps to help Cole get his medication — like asking Cole’s doctor to request an exception to OptumRx’s new formulary or approve an alternative medication that was covered by his insurance.
OptumRx responded with a motion to dismiss the federal lawsuit Friday. In a brief supporting the motion, attorneys for OptumRx asserted that while the company “expresses its deepest sympathies to the parents and loved ones of Cole Schmidtknecht, whose untimely death is unquestionably heartbreaking,” federal law protects OptumRx from the claims made in the lawsuit.
The court filing cites the Employee Retirement Income Security Act of 1974, known as ERISA, which it states was enacted by Congress to ensure regulation of employee benefit plans are handled at the federal, and not the state, level. ERISA’s “remedial provisions” are “the sole avenue” for resolving claims that concern employee benefit plans that are governed by ERISA, like the benefit plan Schmidtknecht had through his employer, OptumRx argues.
RELATED: A 22-year-old from Appleton died after his inhaler price skyrocketed. His parents are suing.
OptumRx’s court filing also argues that the facts listed in the lawsuit complaint “present an incomplete picture of the events surrounding Mr. Schmidtknecht’s interactions with the pharmacy, and indirectly with Optum Rx.”
The company claims that despite the lawsuit complaint’s statement that Cole had been taking Advair Diskus regularly up until the medication stopped being covered by his insurance, he “had not filled any prescriptions for Advair Diskus using his OptumRx pharmacy benefit since April 5, 2022.”
The lawsuit remains ongoing. Attorneys for Walgreens filed a motion Friday requesting a time extension to file a response to the lawsuit complaint, according to court records.
“OptumRx has asked that the Court dismiss them from the case before the parties engage in any fact discovery,” Michael Trunk, one of the Schmidtknecht family’s attorneys, said in a statement. “There is no basis in federal or Wisconsin state law for its request, and the Schmidtknechts look forward to litigating the issue before the Court.”
Bil Schmidtknecht previously told the Post-Crescent he hopes the lawsuit can raise awareness about a need for reform of pharmacy benefit managers like OptumRx.
Pharmacy benefit managers, also known as PBMs, are companies that act as intermediaries between drug companies and pharmacies. Most of the largest PBMs are owned by health insurance companies or their parent companies. This means PBMs have significant power over the pharmaceutical supply chain — and can inflate medication prices for Americans, the Federal Trade Commission has warned.
In 2023, the three largest PBMs — CVS Caremark, Express Scripts and OptumRx — processed close to 80% of the approximately 6.6 billion prescriptions dispensed by pharmacies around the United States, according to a 2024 FTC report. The six largest PBMs manage close to 95% of prescriptions in the country.
Contact Kelli Arseneau at 920-213-3721 or karseneau@gannett.com. Follow her on X, formerly Twitter, at @ArseneauKelli.
This article originally appeared on Appleton Post-Crescent: OptumRx asks judge to dismiss lawsuit over Cole Schmidtknecht’s death
#Company #family #Wisconsin #man #died #inhaler #price #jumped #grounds #sue











Leave a Reply